MADRS Score Interpretation: Patient & Clinician FAQs
February 20, 2026 | By Elias Monroe
Understanding your depression symptoms is a journey that requires the right tools. The Montgomery–Åsberg Depression Rating Scale, or MADRS, is one of the most trusted tools used by doctors worldwide. However, seeing a number on a page can be confusing. You might wonder if a specific score is "good" or "bad."
What does your MADRS score actually mean for your mental health?
Patients and clinicians alike often ask: What does my MADRS score really mean? Let’s demystify the results. It’s normal to feel overwhelmed by your score—depression is complex, but tracking your symptoms is a brave first step. This guide helps you navigate the complexities of MADRS results. Whether you are tracking your own progress or managing a patient’s treatment, clarity is essential. We will break down the scoring ranges, compare the tool to other assessments, and explain how to use our online tool to get deeper insights into your well-being.
Understanding Your MADRS Assessment Results
The MADRS scale scores ten items from 0 to 6, totaling 0–60 points. Unlike general mood trackers, it zeroes in on depression's psychological symptoms—a key reason clinicians trust it. This specific focus makes the scale incredibly sensitive to changes in a person's condition.
What Do Different MADRS Score Ranges Actually Mean?
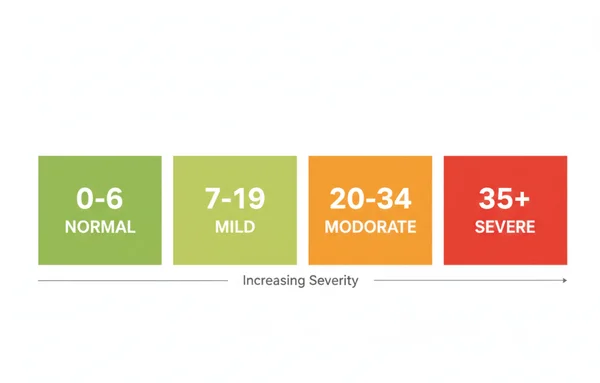
To make sense of a result, it helps to view the score within established clinical brackets. These brackets help determine the severity of depressive symptoms at a specific point in time. While only a professional can provide a diagnosis, these ranges offer a helpful score interpretation for users.
- 0 to 6: Normal or Clinical Remission. A score in this range suggests that the individual is either not experiencing depression or has successfully reached remission through treatment.
- 7 to 19: Mild Depression. This range indicates that symptoms are present and likely causing some distress. However, the individual may still be able to function in daily life with effort.
- 20 to 34: Moderate Depression. At this level, symptoms are often clear. They interfere significantly with work, social life, and home responsibilities.
- 35 and Above: Severe Depression. Scores in this range represent intense suffering and a high level of functional impairment. This often requires immediate clinical intervention.
It is important to remember that these numbers are a "snapshot." They reflect how you have felt over the past week. Because the scale is so precise, even small movements in the score tell a story. They indicate whether a treatment is working or if a new strategy is needed.
How MADRS Scores Compare to Other Depression Assessment Tools
Many patients are familiar with the PHQ-9 (Patient Health Questionnaire) or the Hamilton Depression Rating Scale (HAM-D). You might wonder why a clinician would choose the MADRS over these other options. The answer lies in its design.
The PHQ-9 is excellent for quick screening, but it is less detailed than the MADRS. The HAM-D is very comprehensive but includes many questions about physical symptoms, like insomnia or weight loss. In some cases, physical symptoms can be caused by other health issues. This might "blur" the depression data.
The MADRS was specifically designed to be more sensitive to the core emotional and cognitive aspects of depression. This makes it the "gold standard" for clinical trials and monitoring medication efficacy. If you want a tool that truly measures "mood lift" or "emotional recovery," the MADRS is often the superior choice. Unlike shorter checklists, our online MADRS assessment offers a detailed snapshot of your psychological health—helping you spot patterns faster.
Practical Considerations for MADRS Assessments
Using the MADRS effectively requires more than just taking the test once. It is a dynamic tool designed for monitoring. To get the most out of it, you need to understand the rhythm of assessment and the factors that can influence your results.
How Often Should You Retake the MADRS Assessment?
One of the most common questions from patients is how often they should check their score. There is no single "right" answer, but clinical standards provide some helpful guideposts. If you are starting a new medication or therapy, checking your score every one to two weeks is often recommended.
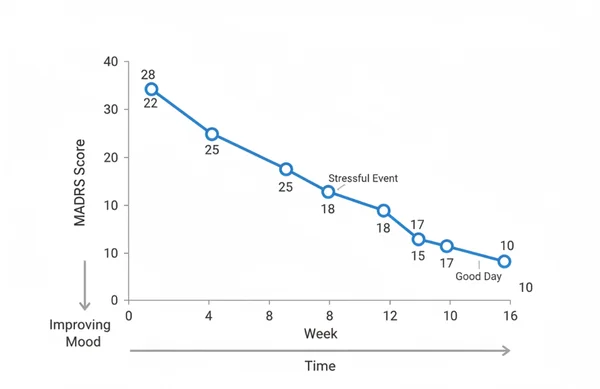
Frequent testing allows you to see the "trend line" of your recovery. Depression recovery is rarely a straight line. It is usually a series of ups and downs. By taking a regular test, you can see if the overall direction is improving. This holds true even if you have a few bad days.
For those in a stable phase of recovery, checking once a month can serve as an "early warning system." If your score creeps from "normal" to "mild," contact your provider. This helps prevent a full relapse. Clinicians often appreciate having this data, as it provides a concrete history of the patient's experience between appointments.
What Causes MADRS Score Fluctuations Between Assessments?
It is natural to feel frustrated if your score goes up after a week of improvement. However, fluctuations are a normal part of the process. Several factors can influence your MADRS score without necessarily meaning your depression is getting worse.
External stressors—like work pressure or family conflicts—often spike MADRS scores for 'inner tension' or 'pessimism.' Physical health issues (e.g., chronic pain) can also raise scores for fatigue or sleep loss.
The time of day you complete the assessment can also have an impact. Some people experience "diurnal variation." This is where symptoms are much worse in the morning but improve by the evening. To ensure your data is as accurate as possible, try to start your test at the same time of day each time. This consistency helps filter out "noise" and shows the true state of your mental health.
MADRS Reports: Understanding Your Results
Once you have completed the ten questions, you receive a total score. We take this a step further by offering an AI-driven analysis. This report helps bridge the gap between a raw number and a meaningful understanding of your condition.
Interpreting Your MADRS AI Report vs. Clinical Evaluation
An AI-generated report is a powerful tool for self-awareness. It can highlight which specific areas are contributing most to your score. For example, it might identify "inability to feel" or "concentration difficulties." This personalized AI analysis can give you the language you need to describe your feelings to a doctor.
However, it is vital to understand that an AI report is not a replacement for a clinical evaluation. A psychiatrist or therapist looks at more than just a score. They consider your medical history, your non-verbal cues, and the context of your life.
Think of the AI report as a "map" and the clinical evaluation as the "guide." The map shows you where you are, but the guide helps you decide which path to take. Combining the data from an online tool with the expertise of a professional is the most effective way to manage depression.
How Reliable Are Online MADRS Assessments Compared to In-Person Evaluations?
The MADRS was traditionally administered by a trained clinician through an interview. However, research has shown that digital versions and self-report versions are highly reliable. In fact, some patients find it easier to be honest when answering questions on a screen.
The digital format removes the "social desirability bias." This is where a patient might downplay their symptoms to avoid worrying their doctor. When you use a trusted platform, the algorithm calculates your score with perfect accuracy. This eliminates human error in math.
As long as the online tool uses the original, validated ten questions, it is a highly reliable method for tracking symptoms. It provides an accessible way for people to monitor their health from the comfort of home. This is especially helpful for those with limited mobility or busy schedules.
Key Takeaways: Turning Your MADRS Score Into Actionable Insights
Understanding your MADRS score is the first step toward better depression management. By knowing what the ranges mean and how the scale compares to other tools, you gain a sense of control over your mental health journey. Remember that a single score is just one piece of the puzzle. The real value of the MADRS lies in its ability to track your progress over time. It highlights the specific areas where you need the most support.
Whether you are monitoring treatment progress or seeking initial insights, regular assessments provide valuable clarity. These insights allow for more productive conversations with your doctor. They also lead to more informed decisions about your care.
Ready to take your first assessment or explore your results further? Use our clinical assessment tool today to access your personalized AI analysis. Taking ten minutes today can provide the clarity you need for a better tomorrow.
FAQ Section
Can my MADRS score be influenced by factors other than depression symptoms?
Yes. While the MADRS focuses on core depressive symptoms, external factors can play a role. Physical illness, significant life stress, or severe sleep deprivation can increase your scores. Items like "lassitude" or "reduced sleep" are often affected. It is always best to note any major life events when you review your score results with a professional.
What should I do if my MADRS score changes significantly between assessments?
A significant change—usually 5 points or more—indicates a shift in your clinical state. If your score drops significantly, your treatment is likely working well. If it rises, it may be a sign that you need to adjust your medication or therapy. If you see a major jump, we recommend you consult a professional to discuss the potential causes.
How accurate are the AI-generated reports compared to clinician interpretations?
AI-generated reports use the established scoring logic of the Montgomery–Åsberg scale. They are excellent for identifying patterns and providing a clear summary of your current state. While they are highly accurate in reflecting your data, a clinical evaluation is still necessary for a formal diagnosis.
Is there an optimal time of day to complete a MADRS assessment?
To get the most consistent data, you should complete the test at the same time each day. Many clinicians suggest late morning or early afternoon. This helps avoid the "morning dip" or "evening fatigue" that can sometimes skew the results of a mood assessment.
Can family members help interpret a patient's MADRS results?
Family members can be great observers. They might notice changes in "apparent sadness" or "lassitude" that the patient doesn't see. Sharing your MADRS report with a trusted family member can help them understand what you are going through. However, clinical interpretation should always be left to a healthcare provider.