MADRS for Treatment Efficacy: Tracking Depression Progress
The journey through depression treatment can be complex, often feeling like navigating a foggy path. You may be following a treatment plan, but the day-to-day fluctuations in mood can make it difficult to see the bigger picture. The journey to recovery requires a reliable compass, and for many, the MADRS (Montgomery-Åsberg Depression Rating Scale) provides just that. How do you know if you're truly making progress, or if your current intervention is working? This scale offers a clinically trusted, objective tool to shine a light on this path, providing clear indicators for both patients and healthcare professionals. Discover how this powerful scale can be your guide in monitoring treatment efficacy and tracking real progress with a free MADRS assessment.

This guide will walk you through how the MADRS is used for effective treatment monitoring. It’s designed for individuals seeking to understand their journey, as well as for clinicians looking for reliable methods to track patient outcomes. By the end, you'll understand how to leverage this gold-standard tool to bring clarity to the treatment process.
Disclaimer: This article is for informational purposes only. The MADRS is a monitoring tool and not a substitute for professional medical advice, diagnosis, or treatment. Always consult with a qualified healthcare provider regarding your mental health.
Why Monitor Depression Treatment Progress with MADRS?
Simply "feeling better" is subjective and can be misleading. A structured approach is essential for effective depression management. The MADRS provides a standardized framework that quantifies symptom severity, transforming abstract feelings into concrete data that can be tracked over time. This process is crucial for making informed decisions about treatment plans.
The Clinical Need for Objective Measurement
In mental healthcare, objective measurement is fundamental to evidence-based practice. While patient narratives are invaluable, they can be influenced by recent events or mood shifts. A standardized assessment tool minimizes this variability by assessing ten specific domains of depression, including apparent sadness, inner tension, and concentration difficulties.
This objectivity creates a common language between patients and clinicians. When a score decreases from 32 to 20 over several weeks, it provides a clear, quantifiable signal of improvement that both parties can understand and discuss. This data-driven approach allows healthcare providers to confidently assess whether a specific medication, therapy, or lifestyle change is having the desired effect, enabling timely adjustments to the treatment plan. A consistent assessment tool helps to ensure that progress is real and sustainable.
Empowering Patients Through Self-Assessment & Insight
Monitoring isn't just for clinicians; it's a powerful tool for personal empowerment. Engaging in regular self-assessment gives you an active role in your own recovery. By using a MADRS self-report, you can develop a deeper insight into your own patterns. You might notice, for example, that your sleep quality scores improve before your mood scores do, providing early signs of progress that might otherwise be missed.
This process fosters a sense of agency and control. Instead of feeling like a passive recipient of care, you become a collaborative partner in your mental health journey. Documenting your scores over time allows you to bring concrete data to appointments, leading to more productive and focused conversations with your doctor or therapist. You can confidently say, "My score has dropped by eight points, and I've seen the biggest improvements in these specific areas." You can take the MADRS test to start gaining these insights.
How the MADRS Scale Aids Treatment Efficacy Tracking
The core strength of the MADRS Scale lies in its sensitivity to change. It was specifically designed to be more responsive to the effects of antidepressant treatments than other scales. This makes it an ideal instrument for treatment efficacy tracking, helping to determine not just if a patient is getting better, but by how much.
Understanding MADRS Scoring for Progress Evaluation
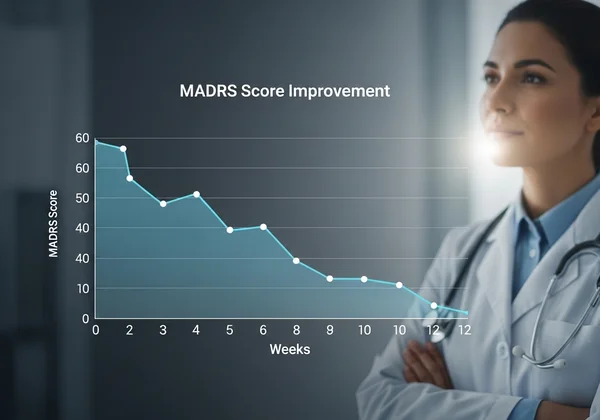
The MADRS consists of 10 questions, each scored on a scale from 0 to 6, leading to a total score between 0 and 60. A higher score indicates more severe depression. For progress evaluation, the focus is not on a single score but on the trend over time. A baseline score is typically established before a new treatment begins. Subsequent assessments are then compared to this baseline.
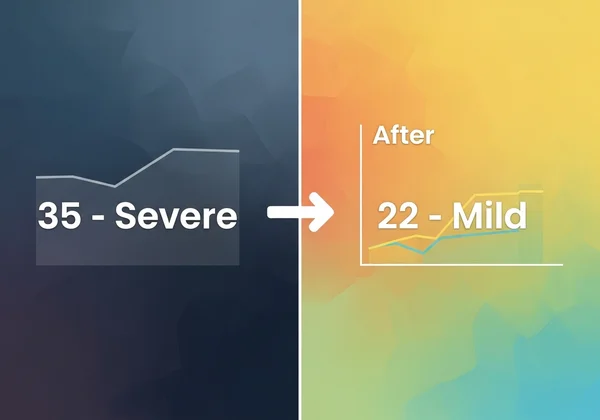
A significant reduction in the MADRS scoring total suggests that the treatment is working. For instance, a patient might start with a score of 35 (severe depression). After four weeks of treatment, a new score of 22 (mild-to-moderate depression) indicates a positive response. This numerical feedback is far more precise than relying solely on a general feeling of improvement, providing a clear metric for ongoing assessment.
Identifying Meaningful Clinical Change and Response
In clinical trials and practice, specific thresholds are used to define treatment response. Generally, a 50% or greater reduction in the MADRS score from baseline is considered a positive response. Remission, which is the ultimate goal of treatment, is often defined by a score falling below a certain cutoff, typically 10 or less.
Identifying this clinical change is vital. It confirms that the current treatment strategy is effective and should be continued. Conversely, a lack of significant change after an adequate trial period may indicate that the treatment is not working as expected. This data empowers clinicians to make evidence-based decisions, such as adjusting a medication dosage or exploring a different therapeutic approach, ensuring the patient is always on the most effective path toward recovery.
Practical Application: MADRS for Ongoing Assessment
The true value of the MADRS assessment is realized through its consistent and practical application. It serves as a dynamic tool for mental health follow-up, adaptable for both professional clinical settings and individual self-monitoring. Integrating it into a regular routine provides a continuous stream of data that illuminates the path to wellness.
For Professionals: Integrating MADRS into Clinical Practice
For psychiatrists, therapists, and general practitioners, the MADRS clinical tool is an invaluable asset for streamlining patient monitoring. Integrating regular MADRS assessments into appointments—for instance, at baseline, 2 weeks, 4 weeks, and 8 weeks—creates a structured dataset for each patient. This facilitates efficient and effective consultations, as the discussion can be grounded in objective changes.
Modern platforms make this process even simpler. Using an online tool like our platform allows patients to complete the assessment prior to their appointment, saving valuable session time. The results can be quickly reviewed, allowing the clinician to focus on interpreting the changes and discussing the next steps. This approach enhances the quality of care and supports efficient MADRS professional use. You can use our clinical tool to streamline your practice.
For Individuals: Self-Monitoring Your Mental Health Journey
For those on a personal recovery path, the scale serves as a private and empowering tool for depression progress tracking. Setting a regular schedule for self-assessment—perhaps every two weeks—can help you stay connected to your mental state in a structured way. This routine creates a personal health log, revealing patterns that might have otherwise gone unnoticed.
Seeing your score gradually decrease can be incredibly motivating and reaffirming, especially on difficult days. It provides tangible evidence that your efforts are paying off. Conversely, if your score plateaus or increases, it serves as an early warning sign, prompting you to seek support from your healthcare provider. This proactive approach to self-monitoring transforms your role from passive to active in your own wellness.
Leveraging AI Reports for Personalized Treatment Insights
Standard scoring provides the "what," but deeper analysis can reveal the "why." This is where advanced tools add unique value. Our platform offers an optional AI MADRS report that translates your score into personalized, actionable insights. This report goes beyond the numbers to analyze patterns in your responses, highlighting specific strengths and challenges.

For example, the AI MADRS report might identify that while your overall mood has improved, your concentration and motivation scores remain high. This specific insight allows for a more targeted conversation with your provider about strategies to address those particular symptoms. It turns raw data into a narrative for recovery, making it an exceptional tool for anyone seeking a deeper understanding of their treatment journey. You can explore the AI report after completing the test.
Your Path to Effective Depression Monitoring with the MADRS Tool
Tracking the efficacy of depression treatment is no longer a journey in the dark. The Montgomery-Åsberg Depression Rating Scale offers a clear, reliable, and clinically validated method to measure progress for both individuals and their healthcare providers. By translating subjective experiences into objective data, the MADRS empowers informed decision-making, fosters collaboration, and ultimately illuminates the path toward recovery.
Whether you are a clinician seeking an efficient monitoring tool or an individual wanting to take an active role in your mental health, the MADRS is an indispensable ally. We provide a secure, accessible, and user-friendly platform to conduct the MADRS assessment. Take the next step in your journey today by using our tool to gain clarity and confidence in your treatment plan.
Ready to see where you stand? Begin tracking today and take control of your mental wellness journey. We encourage you to share your thoughts or questions about using the MADRS for treatment monitoring in the comments below.
Frequently Asked Questions About MADRS Treatment Monitoring
How often should the MADRS be used to track treatment efficacy?
The frequency of MADRS assessment depends on the clinical context and should be guided by a healthcare professional. A common schedule involves a baseline test before starting a new treatment, followed by assessments every 2 to 4 weeks to monitor initial response. For long-term monitoring, it might be used every few months or during periods of significant life changes to ensure stability.
What do changes in MADRS scores signify during treatment?
Changes in MADRS scores provide a quantitative measure of treatment response. A significant decrease (often defined as 50% or more from baseline) indicates a positive response to the treatment. A small change or an increase may suggest the current intervention is not sufficiently effective, prompting a discussion with your provider about potential adjustments. Remember, the goal is not just a lower score but sustained improvement in overall functioning. For more details, you can begin by understanding your score.
Can this platform assist both patients and professionals in monitoring progress?
Absolutely. Our platform is designed to serve both audiences. For individuals, it offers a confidential and easy-to-use platform for self-monitoring and gaining personalized insights through our optional AI reports. For professionals, it serves as an efficient tool to collect standardized data from patients, helping to streamline assessments, track treatment efficacy over time, and facilitate more productive clinical conversations.