Estudo de Caso MADRS: Acompanhamento do Progresso do Tratamento da Depressão
O caminho no tratamento da depressão pode muitas vezes parecer incerto. Dias de clareza podem ser seguidos por momentos de dúvida, dificultando a avaliação se você está realmente avançando. O progresso pode ser sutil e difícil de medir apenas pelos sentimentos. O que é a escala MADRS? É uma ferramenta clinicamente confiável, projetada para proporcionar objetividade a essa jornada. Este estudo de caso hipotético de "Sarah" ilustra como uma ferramenta estruturada, como a Escala de Avaliação de Depressão de Montgomery-Åsberg (MADRS), oferece uma abordagem clara e baseada em dados. Ela capacita indivíduos e clínicos a monitorar mudanças nos sintomas e avaliar a eficácia do tratamento ao longo do tempo. Descubra como você pode obter clareza semelhante em seu próprio caminho usando nossa avaliação MADRS gratuita.
Apresentando Sarah: Avaliação Inicial e Metas de Tratamento
Conhecemos Sarah, uma designer gráfica de 32 anos, quando ela decide procurar ajuda para um estado de ânimo decaído persistente, falta de energia e perda de interesse em seu trabalho criativo. Seu médico sugere o uso da escala MADRS para estabelecer uma compreensão inicial de seus sintomas. Este passo inicial é crucial, pois fornece um ponto de partida em relação ao qual todo o progresso futuro pode ser medido. Ele transforma uma sensação vaga de sentir-se indisposta em uma pontuação quantificável.
O que é a Escala MADRS? Compreendendo as Pontuações de Base
A Escala de Avaliação de Depressão de Montgomery-Åsberg (MADRS) é um questionário diagnóstico de dez itens usado por clínicos para medir a gravidade de episódios depressivos. Cada item, que abrange sintomas como tristeza manifesta, tensão interna e dificuldades de concentração, é pontuado de 0 a 6. Sarah senta-se para fazer o teste em nossa plataforma online. O processo é simples e leva apenas alguns minutos. Sua pontuação inicial é 31, o que a coloca no nível de "depressão grave". Embora o número seja preocupante, também é um fator confirmador. Ele dá um nome e um peso ao que ela tem experimentado, fornecendo uma base sólida para sua jornada de saúde mental.

Definindo um Caminho: Plano de Tratamento e Expectativas Iniciais de Sarah
Com uma linha de base clara, Sarah e seu profissional de saúde criam em conjunto um plano de tratamento. Ele inclui sessões semanais de terapia e o início do tratamento com um medicamento SSRI. O objetivo não é magicamente zerar sua pontuação da noite para o dia, mas ver uma redução gradual e constante nas próximas semanas e meses. Eles concordam que Sarah usará o teste MADRS online semanalmente para monitorar seu progresso. Este acompanhamento regular cria uma rotina estruturada para monitorar a eficácia do tratamento e facilita conversas mais produtivas com sua terapeuta e médico.
Monitorando o Progresso: Como as Pontuações MADRS Refletem a Mudança ao Longo do Tempo
O verdadeiro poder da escala MADRS é demonstrado quando ela é usada de forma consistente. Para Sarah, suas pontuações semanais tornam-se um mapa confiável de sua jornada de recuperação. Elas destacam melhorias, identificam desafios e orientam os ajustes necessários em seu tratamento. Ela fornece dados objetivos que complementam seus sentimentos subjetivos, oferecendo uma visão mais completa de seu bem-estar.
As Primeiras Semanas: Identificando Respostas Iniciais com a Ferramenta MADRS Online
Nas primeiras três semanas, as pontuações de Sarah variam. Sua pontuação na segunda semana cai para 28, mas na terceira semana volta a 29. Ela se sente um pouco desanimada, mas olhando mais de perto as pontuações dos itens individuais na ferramenta MADRS, ela e sua terapeuta identificam um ponto importante. Sua pontuação para "fadiga" (uma sensação de cansaço) melhorou consistentemente, mesmo que sua pontuação de "tensão interna" permaneça alta. Essa análise detalhada de seu monitoramento de sintomas regular mostra que o tratamento está tendo um efeito positivo, mesmo que a sensação geral ainda não seja de alívio completo.
Insights de Meio de Tratamento: Reconhecendo Platôs, Recaídas e Ajustes
Por volta dos dois meses, o progresso de Sarah parece estagnar. Sua pontuação MADRS permanece em torno de 22 por algumas semanas, indicando depressão moderada. Ela se sente melhor do que quando começou, mas uma sensação de estar "presa" se instala. É aqui que os dados objetivos do MADRS se tornam cruciais. Ao apresentar essas pontuações consistentes ao seu médico, eles decidem fazer um ajuste sutil na dosagem de sua medicação. Essa decisão não se baseia em um único dia ruim, mas em um padrão claro revelado através do rastreamento consistente da evolução da pontuação MADRS. Você pode descobrir seus resultados e rastrear seus próprios padrões com nossa ferramenta.
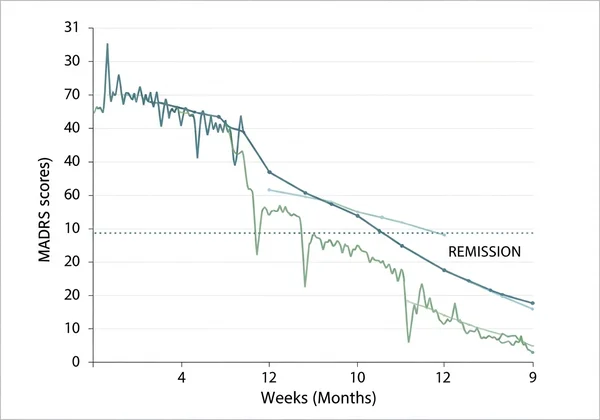
Melhora Sustentada: Confirmando a Remissão e Mantendo o Bem-estar
Nos meses seguintes, a pontuação de Sarah começa uma redução constante. Aos seis meses, ela obtém uma pontuação de 9, colocando-a na categoria de remissão. Este marco é uma poderosa confirmação de seu trabalho árduo e da eficácia de seu plano de tratamento. Ela decide continuar fazendo a avaliação MADRS mensalmente, não por medo, mas como uma ferramenta proativa para manter seu bem-estar. Isso a capacita a permanecer atenta à sua saúde mental e a identificar quaisquer possíveis recaídas antes que se tornem grandes contratempos.
Além dos Números: Relatórios de IA da Nossa Plataforma para Insights Mais Profundos
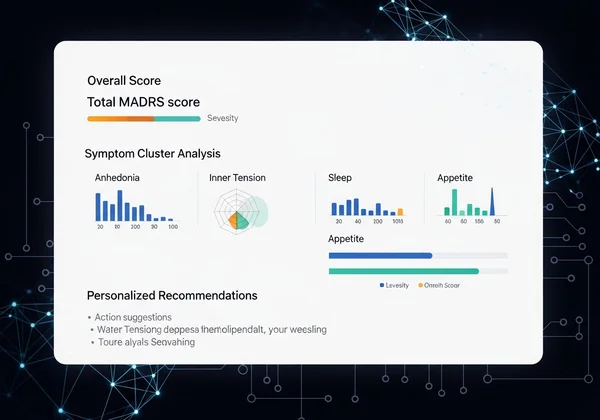
Embora o acompanhamento da pontuação MADRS forneça dados essenciais, compreender a história por trás dos números pode permitir um avanço adicional. Nossa plataforma oferece um relatório opcional, baseado em IA, que transforma uma pontuação numérica em uma narrativa personalizada com conselhos acionáveis. Sarah opta por receber seu relatório para ter uma compreensão mais rica de seus resultados.
Como a IA Decodifica os Resultados MADRS: Análise de Padrões e Agrupamentos de Sintomas
A análise de IA vai além de interpretar uma única pontuação. Ela analisa os padrões particulares nas respostas de Sarah. Por exemplo, ela destaca que seus desafios estão principalmente relacionados à anedonia (interesse reduzido) e tensão interna, enquanto seu sono e apetite permaneceram relativamente estáveis. Isso a ajuda a focar suas estratégias terapêuticas em áreas específicas. Este nível de detalhe fornece insights personalizados que vão muito além de uma mera pontuação total, tornando sua recuperação mais direcionada.
Capacitando a Ação: Recomendações Personalizadas da Sua Análise de IA
A parte mais valiosa do relatório de IA para Sarah é a seção "Recomendações Práticas". Com base em seu perfil de sintomas individualizado, o relatório sugere estratégias concretas e baseadas em evidências. Para seus desafios com a anedonia, ele recomenda planejar pequenas atividades prazerosas. Para abordar a tensão interna, ele sugere exercícios de mindfulness e temas para diário. Essas não são dicas genéricas; são adaptadas aos seus resultados específicos do MADRS, tornando-as relevantes e fortalecedoras. Este recurso ajuda a preencher a lacuna entre a avaliação e a ação, um passo fundamental em qualquer processo de cura. Para ver quais insights você pode descobrir, inicie sua avaliação hoje.
Sua Jornada para a Clareza, Capacitada pela Ferramenta MADRS
A história de Sarah é um testemunho do poder de combinar orientação profissional com automonitoramento objetivo. A escala MADRS forneceu a ela uma bússola, transformando uma jornada que parecia esmagadora e abstrata em um caminho gerenciável e mensurável em direção à recuperação. Ao rastrear consistentemente seus sintomas, ela foi capaz de celebrar pequenas vitórias, fazer ajustes fundamentados no tratamento e construir confiança em sua capacidade de gerenciar sua saúde mental.
Sua jornada é única, mas a necessidade de clareza é universal. Se você está apenas começando a explorar seus sintomas ou está ativamente em tratamento, usar uma ferramenta clínica confiável pode ser um divisor de águas. Convidamos você a experimentar MADRS.net hoje para dar o primeiro passo. Obtenha uma compreensão mais clara do seu bem-estar emocional, acompanhe seu progresso ao longo do tempo e descubra os insights personalizados que podem impulsionar seu caminho para a recuperação.

Aviso Legal: Este estudo de caso é apenas para fins ilustrativos e não representa um indivíduo real. MADRS.net é uma ferramenta informativa e não substitui aconselhamento médico profissional, diagnóstico ou tratamento. Sempre procure o conselho de seu médico ou outro profissional de saúde qualificado com qualquer dúvida que possa ter sobre uma condição médica.
Perguntas Frequentes Sobre o Monitoramento e Tratamento MADRS
Posso usar o MADRS para automonitoramento para acompanhar meu tratamento de depressão?
Sim, absolutamente. Embora o MADRS tenha sido projetado para uso clínico, é uma excelente ferramenta para automonitoramento para monitorar seus sintomas entre as consultas. O uso de nossa plataforma permite que você monitore consistentemente sua pontuação e compartilhe esses dados valiosos com seu profissional de saúde, levando a conversas mais informadas e colaborativas sobre seu plano de tratamento.
Qual a precisão da escala MADRS no monitoramento do progresso do tratamento?
O MADRS é considerado um "padrão ouro" em ambientes clínicos por sua alta sensibilidade às mudanças nos sintomas depressivos. É altamente confiável e válido para monitorar a resposta ao tratamento ao longo do tempo. Sua precisão reside em sua capacidade de quantificar as mudanças nos principais sintomas depressivos, fornecendo uma medida objetiva para complementar seus sentimentos e experiências pessoais.
Qual a diferença entre as pontuações MADRS que indicam melhora versus recaída?
A melhora é tipicamente mostrada por uma redução constante em sua pontuação total MADRS ao longo do tempo. Uma redução de 50% ou mais em relação à sua pontuação de ponto de partida geralmente indica uma resposta significativa ao tratamento. Por outro lado, uma recaída pode ser indicada por um aumento sustentado em sua pontuação após um período de remissão ou melhora, sugerindo um retorno de sintomas significativos. O monitoramento regular ajuda a identificar essas tendências precocemente.
O uso de nossa ferramenta de monitoramento MADRS para tratamento é gratuito?
Sim, a avaliação MADRS principal em nossa plataforma é totalmente gratuita. Você pode fazer o teste de 10 perguntas e receber sua pontuação instantaneamente sem nenhum custo. Também oferecemos uma análise opcional e aprofundada, baseada em IA, mediante uma taxa, que fornece os insights personalizados e sugestões práticas discutidos no estudo de caso. Você pode fazer a avaliação gratuita a qualquer momento.
Como os clínicos geralmente usam as pontuações MADRS para ajustar os planos de tratamento?
Os clínicos usam as pontuações MADRS como pontos de dados objetivos para orientar a tomada de decisões clínicas. Se a pontuação de um paciente não estiver melhorando após um período de tratamento adequado com um tratamento específico, um clínico pode considerar ajustar a dosagem da medicação, mudar o tipo de terapia ou explorar outras intervenções. As pontuações os ajudam a determinar se um tratamento é eficaz, parcialmente eficaz ou ineficaz, garantindo que o plano seja sempre otimizado para a recuperação do paciente.